The Global Compact for Migration and Public Health in the Context of the Covid-19 Pandemic
Untapped Potential for Strengthening Health Systems
SWP Comment 2020/C 44, 29.09.2020, 4 Pagesdoi:10.18449/2020C44
Research AreasThe Covid-19 pandemic has made policy-makers aware of the challenges of maintaining quality health care in times of crisis. Strengthening health systems is the key to meeting these challenges. The implementation of the Global Compact for Safe, Orderly and Regular Migration (GCM), agreed in December 2018, can make an important contribution in this respect. A comparison of the GCM objectives with the basic pillars of health systems defined by the World Health Organization (WHO) shows what this contribution could look like. There are many synergies and opportunities for action. The health policy potential of the GCM lies specifically in improving access to health services and meeting the demand for health professionals.
Since early 2020, efforts to contain the Covid-19 pandemic have dominated the international agenda. This has also shaped current migration policy. Many governments are seeking to reduce cross-border mobility in order to slow the spread of the virus and interrupt chains of infection. This can be useful in the short term. However, those who restrict the debate about the interdependencies between migration and the pandemic to the need to limit mobility fail to recognise the health policy potential of migration policy instruments that, instead of reducing migration, aim to improve the conditions under which it takes place. The implementation of the GCM can make an important contribution, both towards curbing the current spread of infections and preventing future pandemics.
Health Risks Resulting from Inadequate Migration Policy
The Covid-19 pandemic highlights the health risks associated with poor migration policy decisions. These include the risks associated with the precarious housing and working conditions of many migrants and refugees. Examples from the German meat and agriculture industries show that numerous chains of infection can be directly attributed to inadequate hygiene measures and the cramped accommodations of seasonal workers. Similar problems exist in group accommodation settings and refugee camps, which often pose health risks for the residents and where infections can spread quickly.
Moreover, refugees and migrants often do not have sufficient access to health care. This problem is particularly pronounced among undocumented migrants, who often fear the data collection process associated with the use of health services. The fact that chains of infection are difficult or impossible to trace in the case of irregular migration poses additional challenges for transit and destination countries.
Finally, the pandemic reveals two further problems: firstly, how much health care and the stability of the health systems of many wealthy countries depend on cross-border labour migration, and secondly, the risks of poaching health care professionals in countries of origin.
The Health Potential of the Global Compact for Migration
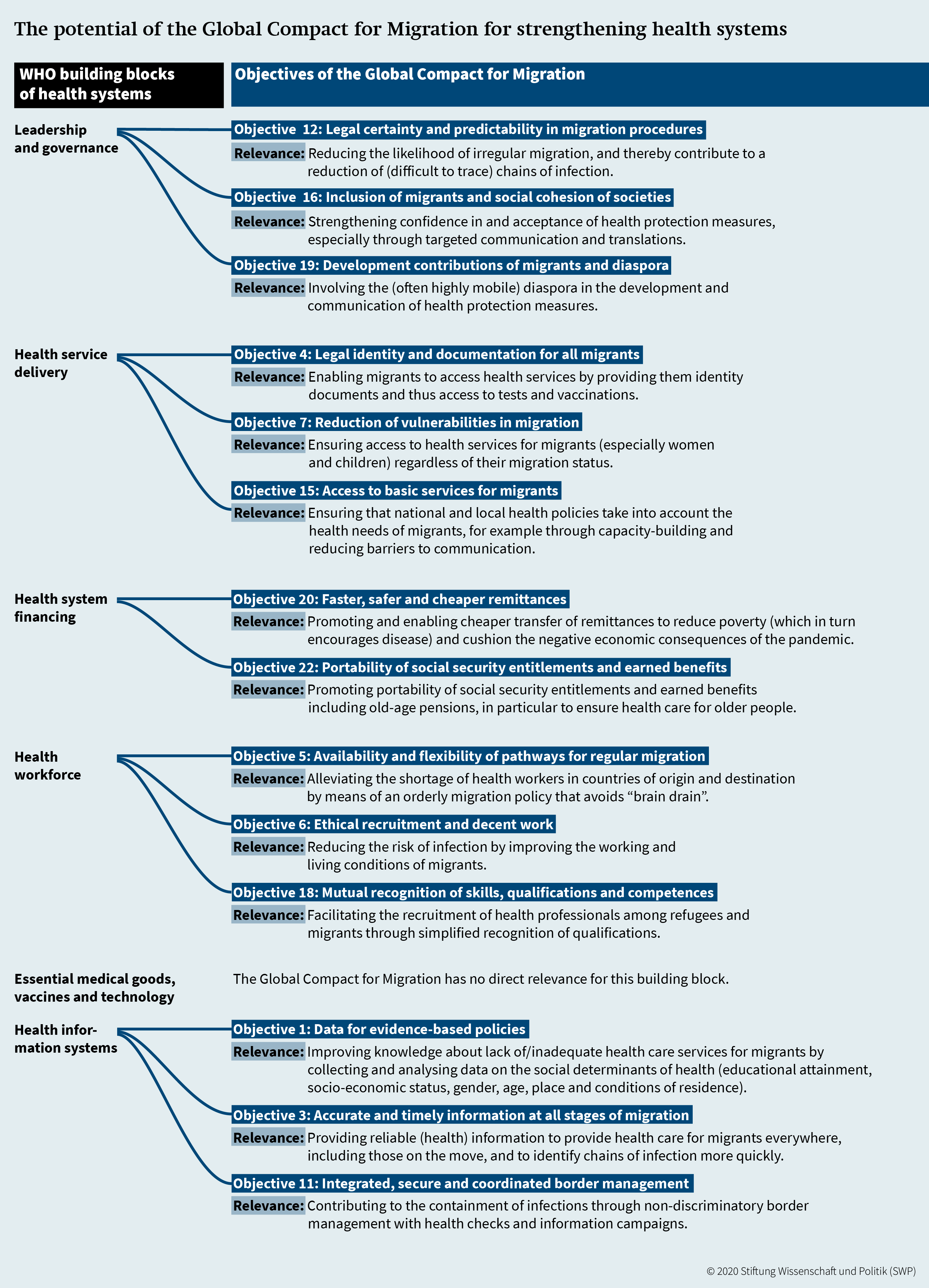
WHO defines public health as “the art and science of preventing disease, prolonging life and promoting health through the organized efforts of society”. According to WHO, health systems – the totality of actors and activities that promote, restore, or maintain public and individual health – are based on six pillars: (1) leadership and governance, (2) health information systems, (3) health system financing, (4) health workforce, (5) medical products, vaccines and technologies, (6) service delivery. To strengthen health systems, these sub-sectors must be made more effective, efficient and equitable, both individually and in their functional interaction. A comparison of WHO’s basic pillars with the 23 objectives of the GCM shows a significant overlap between the two instruments: The latter contain numerous health-related measures whose implementation could strengthen health systems in countries of origin, transit and destination. Figure 1 provides an overview of the objectives listed in the GCM that offer concrete opportunities for action to strengthen health systems.
Recommendations for German and European Policy
According to the comparison, the implementation of the GCM can contribute to five of the six pillars defined by WHO. In the area of leadership and governance, the aim is, among other things, to reduce the likelihood that migration activities will become irregular by strengthening the legal security of migration projects and strengthening migrants’ confidence in health protection measures. Improving the conditions for remittances and the portability of social security entitlements acquired abroad can contribute to the financing of health systems. Progress in the collection and analysis of socio-economic migration data would fill gaps in health information systems, which is crucial for the proper functioning of health systems. However, implementing the GCM would have a particularly strong impact on strengthening the health workforce and improving health service delivery.
Health professionals are the backbone of any health system. Recent studies have shown how indispensable the work of migrant nurses and doctors is in many European countries. In order to meet the demand for these workers, and at the same time avoid a brain drain in the health sector in their countries of origin, a critical review of current recruitment practices and a new impetus to manage labour migration in the health sector are needed. In this respect, Objectives 5 and 6 of the GCM – promoting regular migration routes and the ethical recruitment of labour – can be helpful. Global Skill Partnerships, which are designed to meet the workforce needs of both the countries of origin and the destination countries, constitute a promising development policy approach. In the context of the Covid-19 pandemic, many countries have already started to simplify the accreditation process for the medical and nursing qualifications of migrants and refugees, as suggested by
Objective 18 of the GCM; ensuring that these initiatives lead to permanent changes would further increase the future performance and resilience of health systems.
Access to health services is not just a human right – there is no alternative if the aim is to effectively contain the pandemic. This is the only way to track new infections, prevent them from spreading, and treat pre- and post-pandemic diseases. Objective 4 of the GCM (provision of identity documents), Objective 7 (reducing vulnerabilities in migration) and Objective 15 (ensuring migrants’ access to basic services) offer important suggestions for coming closer to the goal of universal health coverage. Both within Germany and in the context of development cooperation, the Federal Government should endeavour to remove the practical and legal obstacles that are preventing migrants and refugees from accessing health services.
Conclusion
To halt the further spread of Covid-19, many governments will continue to impose mobility and migration restrictions. This may be appropriate in the short term, depending on the situation. Of particular importance, however, is the strengthening of health systems, and the GCM can provide an important impetus for this. The interdependencies between migration and health that have become apparent in the context of the Covid-19 pandemic create scope for action that goes beyond the realisation of the individual objectives of the GCM. An example is the institutional interlinkage between the two policy areas: Health experts should be increasingly involved in the implementation of the GCM and in the international bodies that take decisions on migration issues. Conversely, the same applies to the involvement of migration experts in pandemic management. There are many opportunities for concrete cooperation – at the local level in vocational training and further education within the framework of hospital partnerships; and at the international level in the cooperation of WHO with other international organisations on employment policies in the health sector.
The Covid-19 pandemic has revealed the interdependence of public health with other policy areas. A prudent and forward-looking migration policy that takes into account health-related considerations can strengthen health systems and help to ensure that quality health care is available to all, even in crisis situations.
Dr Steffen Angenendt is Head of the Global Issues Division; Nadine Biehler, Dr Anne Koch and Maike Voss are Associates in the Global Issues Division.
This report was written within the framework of two projects funded by the Federal Ministry for Economic Cooperation and Development: “Flight, Migration and Development – Challenges and Opportunities for Action for German and European Policy” and “Global Health: Challenges and Opportunities for Action to Achieve the Health-related Sustainable Development Goals (SDGs) for German Global Health and Development Policy”.
© Stiftung Wissenschaft und Politik, 2020
All rights reserved
This Comment reflects the authors’ views.
SWP Comments are subject to internal peer review, fact-checking and copy-editing. For further information on our quality control procedures, please visit the SWP website: https://www.swp-berlin.org/en/about-swp/ quality-management-for-swp-publications/
SWP
Stiftung Wissenschaft und Politik
German Institute for International and Security Affairs
Ludwigkirchplatz 3–4
10719 Berlin
Telephone +49 30 880 07-0
Fax +49 30 880 07-100
www.swp-berlin.org
swp@swp-berlin.org
ISSN 1861-1761
doi: 10.18449/2020C44
(English version of SWP‑Aktuell 75/2020)